





By Dr. Arnab Datta
Posted on April 16, 2020
These are unprecedented times in the modern world. It is unprecedented that every person in the world has been affected by Covid 19 some way. In a time like this, we must understand what we can control and what we cannot. Thus I am reminded of the serenity prayer which is not only used in Alcoholics Anonymous and Biblically, but also in many other settings.
“Grand me the serenity to accept the things I cannot change, the courage to change the things I can, and the wisdom to know the difference.”
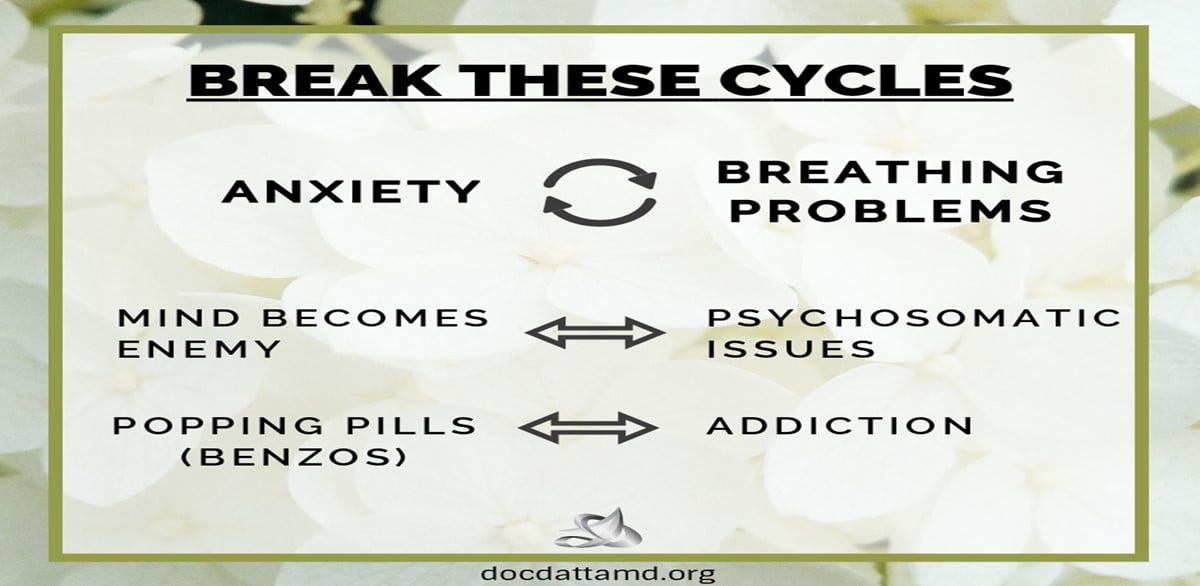
This statement is not only religious, but pervades and transcends religion because it is speaks to human values and speaks to varying mentalities, beliefs, traditions and religions. It is a psychological exercise that can free us from anxiety and fear from what we cannot control. Many people are becoming very anxious and fearful now due to uncertainty. This article is an illustration of how anxiety can lead to breathing and respiratory problems (and vice versa), other manifestations of anxiety and what we can do to flatten the curve when it pertains to these issues.
Firstly, anxiety and panic attacks may be connected to breathing and respiratory problems and vice versa. When people have panic attacks, they breathe more quickly. Most people don’t know why their panic attack starts, as it is often an unconscious phenomenon. It may begin with fear, perhaps triggered by a past or recent traumatic event. For example, someone experiencing a panic attack may have failed an exam, had a car accident, or experienced the death of a loved one.
Secondly, people sometimes have respiratory problems such as asthma, emphysema and chronic obstructive pulmonary disease (COPD). Most people do not see a doctor in the beginning stages of their asthma attack. Later, patients are typically prescribed breathing treatments such as an albuterol nebulizer if their asthma symptoms become more serious, and even stronger treatments for emphysema and COPD. Smoking of any kind, whether they are cigarettes, Juuls/Vapes, or even smoking marijuana can make these respiratory problems worse because smoking irritates the respiratory tract.
Thirdly, at a grassroots level, if someone catches the common cold or flu they might get a runny nose, cough, and some nasal congestion. These are symptoms of an upper respiratory tract infection. Once this infection travels deeper down the respiratory tract it becomes a lower respiratory tract infection. Pneumonia is a serious lower respiratory tract infection caused by a bacteria, virus or fungus. Both upper and lower respiratory tract infections can cause breathing difficulty.
Thus, a person who had these respiratory problems first can become terrified that they are having another respiratory attack. So much so that their respiratory attack can feel like a panic attack. Also, it can be difficult for a doctor difficult to distinguish between the two. In these cases, the doctor often has to obtain collateral information (speak to the patient’s family or friend, that is if the patient does not know) to differentiate which came first, the panic attack or the respiratory problem. This is often times a chicken and egg scenario. That’s why self-understanding and self-monitoring is so important in psychology and in life. People with respiratory problems need to know when they are having a breathing problem and how to stay calm and react correctly before they have a panic attack. Subsequently, people who have a tendency to have panic attacks need to know how to quell their panic attack and not have it manifest as a respiratory problem. There is a scientific statistical correlation between the two and there are psychological centers that dedicate part of their work to the overlap of these two phenomena. These people need the correct treatment for what they are really suffering from. Whether that is medical or mental or both. The remainder of this article speaks of other psychological misunderstandings that occur as a manifestation of fear and anxiety. This is a topic worth discussing because it leads to much misunderstanding and miscommunication between the patient and doctor. Most importantly it impedes the patient’s genuine self-realization and impedes the doctor’s genuine effort to understand the patient.
Some patients are prescribed medications to reduce their anxiety. This can be a selective serotonin reuptake inhibitor (SSRI) such as Prozac, Zoloft or Celexa. These medications can improve both depression and anxiety however they can have a different effect patient by patient. However, that is not the scope of this article. Some patients are prescribed a benzodiazepine such as Klonopin or Valium. Xanax is a short acting benzo that happens to be more addictive than the rest of the benzo family. As a result, psychiatrists try to prescribe less Xanax. During a time of panic, certain patients may want to consume more benzodiazepines than prescribed. They may ask their doctor to prescribe more benzodiazepines before they are due. A benzodiazepine is a controlled substance medication and is regulated by federal organizations, such as the BNE (Bureau of Narcotics Enforcement) and the DEA (Drug Enforcement Agency). This is why patients sign a contract (Patient Agreement) with their doctor stating that controlled substance medication like benzos cannot be refilled before they are due. Patients may have noticed that pharmacies also pay attention to this due date when it comes to controlled substance medications. If a doctor prescribes certain controlled substance medication prescriptions before they are due, then the doctor can lose their license to practice medicine. This unfortunate circumstance can happen when a doctor repeatedly prescribes high doses of controlled substance medication prescriptions before their due date. However, the patient can argue that they were feeling very anxious and found the need to take this medication. As you can see, this is a dilemma between the prescriber and the patient and can certainly ruin the therapeutic relationship between the two. That is why it is important for patients to have more psychotherapy, even over video chat, when they are feeling more anxious. The psychotherapy sessions are very important in uncovering the deeper psychological reasons as to why the patient is feeling anxious. The psychotherapy sessions can help get to the root of why the feel the need to consume their controlled substance medications, such as benzodiazepines. Certain traumas, loss, uncertainties, grievances, and bad relationships may come up in the psychotherapy session. This is important, and often the patient will feel relieved afterwards. Like psychotherapy, meditation may also offer a path for the patient to cope with underlying anxieties. Daily meditation is very helpful in helping a patient let go of things they may be unconsciously holding on to. I believe a combination of psychotherapy and meditation can help the patient reduce the impulse to take more medication than their dosage advises. These two modalities when used in together is a great way to take less medications and possibly be medication free. The psychological goal here is for one to become the master of their emotions and feelings. In the real world, medications are often a great tool to get to the level of emotional mastery. There are my psychologists that refute this idea. However, there is no one correct answer for all people since every person is different. I have seen patients go to therapy for a decade and not improve or improve in just small ways. Psychotherapy is a wonderful thing. However, I have seen medications help people where psychotherapy could not. It takes skill for a psychiatrist to understand a patient well enough to utilize a medication to help that patient accomplish something psychologically and emotionally. An important differentiation in mental health is when to utilize meds and when to Not; taking medications if needed for a specific period of time to help patients along their psychological and emotional journey.
At the same time, it is very important for the psychiatrist to be mindful that the patient can be in a vulnerable position. The patient may not have wanted to take their benzodiazepines so quickly, for example. The psychiatrist must empathize with the patient’s emotional state and history. This is not easy for either party because the psychiatrist may want to simply prescribe the extra medication out of empathy, thus risking their medical license. Both the patient and doctor need to work together. Couples therapy techniques come in handy in these situations. The psychiatrist should implement the speaker-listener technique and reiterate the patient’s concerns so that they may feel heard. Certain sacrifices and compromises must be made from both sides in order to remedy this situation sensibly. However, this is easier said than done. Sometimes the therapeutic relationship does sour when controlled substance medications are taken before they are due. That is why doctors require a patient agreement.
Sometimes a patient’s anxiety can make them impulsive, thus resulting in the patient consuming their controlled substances before the due date. A patient’s anxiety can cause them to experience psychosis. This is a step beyond just an anxiety reaction. The patient may become paranoid, delusional, and their behavior erratic. Their cognitive distortions may take a psychotic turn. Patients might start magnifying certain negative characteristics so greatly that they experience a bizarre delusion. This may be very difficult for a medical doctor to treat in the emergency room or at an urgent care facility. That medical doctor may have to consult a psychiatrist. Often times in the psychiatric emergency room, certain patients receive a medication called Risperdal (1mg twice-a day). This medication (atypical antipsychotic med) is mostly a dopamine antagonist and brings a patient back to baseline if they are having a psychotic episode. Risperdal can be prescribed by an outpatient psychiatrist as well. A psychologist cannot prescribe medications. Some of these patient cases can be resolved on an outpatient basis entirely. That is, if the psychiatrist is willing to see this type of patient in an outpatient setting. A psychiatrist might ask for that patient’s family to be present in the emergency room, depending on the level of patient’s severity. However, I am writing this to explain that sometimes Risperdal is prescribed in an outpatient visit. Thus, patients can and should utilize primary care doctors and mental health providers, even remotely over video chat, before going to the emergency room or urgent care facility.
It can be challenging for a doctor get to the underlying reason why a patient is feeling anxious and panicky or to realize whether a patient is experiencing psychosomatic symptoms. For example, medical doctors usually rule out any medical reasons for the breathing difficulty. If there is no medical explanation, then the medical doctor may say that the cause of anxiety is psychosomatic. “Psychosomatic” is a scientific way of saying “it is all in your head.” Patients do not like hearing that, as it sounds like an insult. It is not an insult when it comes from a medical doctor. The medical doctor has done the necessary work to rule out all medical conditions that may be the cause, and is directing the patient to look for psychological causes. Enter the psychiatrist or psychologist.
It is the psychiatrist or psychologist’s duty to help the patient understand where this anxiety is coming from. It may be affecting the patient significantly in terms of breathing problems. However, the underlying reason in psychosomatic cases is much more nuanced. Firstly, it is difficult for a mental health professional to say that something is psychosomatic. Secondly, the psychiatrist needs the medical doctor’s conclusion that all medical conditions have been ruled out. That is the most helpful information for the psychiatrist. Thirdly, the psychiatrist will proceed to learn about the patient’s life and experiences. Fears, anxieties, trauma, loss, and breakups are discussed in the psychiatric evaluation and the follow up appointments. Fourth, it is somewhat challenging for the patient to talk about things that have been locked away in the deepest vaults of their heart or their consciousness. Fifth, depending on the psychiatrist’s level of skill and vision, they can make the interpretation that the patient is having a psychosomatic reaction. Sixth, this is often insulting and confusing for the patient to hear because these psychosomatic reactions are coming from their unconscious mind. Therefore, it is not an easy to reach, it takes time to reach and it’s not easy to fix. The patient actually has to make more of an effort than the doctor in fixing their psychosomatic problem. The doctor helps the patient understand it (the psychosomatic problem) and guides the patient. It is the patient who has to change their life and habits on a daily basis to free themselves from their psychosomatic problem.
In order to remedy psychosomatic symptoms, the patient must continue speaking with the psychiatrist in ongoing sessions. Talking about repressed loss or trauma brings it (this unconscious element; the origin of the psychosomatic problem) to the conscious mind. Some psychoanalysts believe that once an unconscious thought is brought to the conscious mind their job is done, the patient is cured. That is the best case scenario, and it is great if the patient is cured with just that. However, that is often not the case and the patient continues to suffer from that unconscious trauma. At this point, CBT (cognitive behavioral therapy) might be needed. CBT is a goal oriented psychotherapy that helps the patient establish concrete goals so that they may overcome their anxiety.
It is critical to differentiate these psychological variations of anxiety during this Covid-19 phenomenon. Biotech companies, universities, and state and federal institutions are working night and day to research the nature of this novel coronavirus; creating accurate and fast diagnostic tools, and completing clinical trials for effective treatments. This is the status as of early April 2020. This virus is still new and we as a society are currently grappling with its medical, sociological, and psychological repercussions. It is important not to make our situation worse by succumbing into the pitfalls of our own anxiety. In order to flatten the curve and not overwhelm hospitals, urgent care facilities, and emergency rooms, it is important to first reach out to your primary medical doctor for their opinion and/or your mental health provider. A lot of patients with mild breathing issues are seen in the emergency room, or at an urgent care facility and encouraged to go home the same day, and not every patient is admitted. Some of these patients are simply having anxiety issues. Some of these patients are having anxiety issues and also have a history of the aforementioned breathing problems. Medical and mental health professionals all must be up-to-date with what Covid-19 looks like in order to guide the public. It is important for the mental health professional to help differentiate anxiety, panic attacks, psychosomatic issues and addiction to benzos to reduce anxiety. The medical doctors need the help of the mental health professionals in this time. We need to work together in order to flatten the curve and utilize hospital resources efficiently for the people who truly need treatment. However, I acknowledge the problem that lies in this differentiation; we are still learning about Covid-19 and its mysterious presentation and manifestation. As a result, it’s even more important for patients, families, friends and doctors to communicate calmly so we can properly understand each other. This is the time to utilize outpatient medical doctors and mental health professionals via video chat.